Non-Hodgkin’s Lymphoma
Chemotherapy for cancer and a method of preventing side-effects
The Banfield Cancer Shirt
The C-Shirt ©
Designed when I was being treated for Non-Hodgkin’s Lymphoma
I have also given a public talk about how I survived heart disease with a vegetarian diet, in which I also mention how I survived cancer . It is now available through iTunes for $0.99 here.
The Banfield Cancer shirt is a T-shirt that I designed to reduce the risk of complications in chemotherapy by reducing the incidence of infection at the CVC insertion site. I designed it while recovering from a stem cell transplant in early 2002. The text was written in August 2004 and was first posted on this webpage on 31-10-05 and updated on 31-3-2011
The contents of this webpage are subject to copyright.
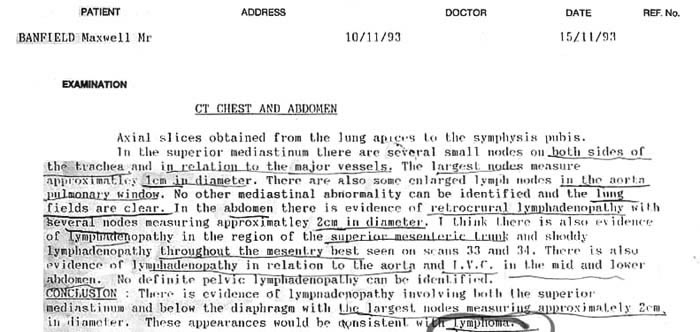
Some background informationI was first diagnosed with a type of cancer called Non-Hodgkin’s Lymphoma in late 1993, and soon after that was told that I had only two months to live with no hope of a cure. The following CAT scan report is dated 10th November of that year. I was told that it was spread throughout my body, my blood, and my bone marrow and had probably been developing for several years. (See more details here) . I am still alive 20 years later, as of 10th November 2013, which probably makes me one of the longest surviving cancer patients in the world. Treatment methods have been improving since 1993, and nowadays the statistics for the five year survival rate of that type of cancer indicate that. . . “Later-stage (111,1V) metastasized disease” is 58.5%. See here. The CAT scan
How I survivedApart from blood tests and CAT scans etc, there were no signs or symptoms until a few years later when I developed a small lump in my neck, and another two years passed when I started to get pain in my chest when I breathed, and then had surgery to remove the lump, and started six months of CHOP chemotherapy. The cancer returned about 18 months later so I had more surgery followed by three months of DHAP chemotherapy, and then spent six weeks in hospital for a stem cell transplant, and Mabthera chemotherapy. A few months after that I was told that the chemo had permanently damaged my immune system, and four years later ended up in hospital again to be treated for an infection and dehydration. Some time later I had a blood test in relation to shoulder surgery, and was told that my immune system was normal. I haven’t had any problems since. During that time I had a lot of problems with side-effects and was always looking for ways of preventing or minimising them. One of the problems occurred when I rolled over in bed and the neck of my standard T-shirt dragged on a tube in my chest and dislodged it, causing leakage and infection which required it to be removed. The tube supplied chemicals, antibiotics, and nutrients into my blood stream, and when it couldn’t be replaced I was advised that there were alternative ways of supplying the chemicals and antibiotics, but not the intravenous nutrients, and that my chances of long term survival without them were significantly reduced. I therefore designed a T-shirt with a neckline that wouldn’t drag on the tube, just in case the cancer relapsed again and I had to have another stem cell transplant in the future. M.B. |
Introduction
During my treatment for Non-Hodgkins lymphoma (a form of cancer) I had a stem cell transplant. Prior to that a CVC tube was inserted into my chest just below my right collarbone and then secured by stitches. It would tend to drag on the neck of my T-shirt when I rolled over in bed and often became entangled. It eventually became loose and leaked, and then infection followed, so it had to be removed. To help prevent that problem I have designed a C-Shirt which I will wear if I have to undergo the same treatment again. That type of T-shirt would significantly reduce the various risks associated with the treatment, and would therefore be a cheap and practical product for other patients to use.
Any company who wishes to manufacture the C-shirt under licence is invited to contact me via email to banfieldm44@gmail.com Similary, parents and friends of cancer patients who wish to use the C-shirt for fund raising purposes can also contact me via the same email address.
 |
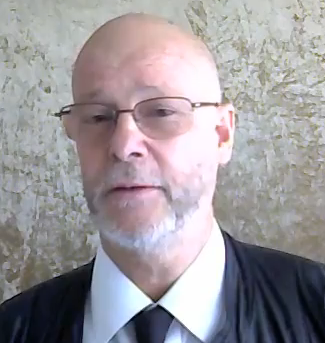
Max Banfield
I am bald, and have thin eyebrows because of more than six years of cancer between 1993 and 2000.
In 1998 my hair became thin during 6 months of CHOP chemotherapy.
In 1999 the cancer returned and it became thinner but grew back.
Soon after, in 2000, I had a stem cell transplant, and went bald. My hair returned, but was thin and sparse, so I keep it shaved.
I then had four years of side-effects but have since made a complete recovery.
In December 2000 I entered hospital to be given a stem cell transplant and chemotherapy for the treatment of a form of cancer called Non-Hodgkins Lymphoma.
Before the treatment started I was taken to a clinic where a surgeon was to insert a tube into my chest. This tube was called a central venous catheter or CVC. As I laid on a bed a nurse brought in a package sealed in plastic. When the surgeon unwrapped it he withdrew a cleaned and sterilised cotton surgical gown and mask and plastic gloves. He then opened another sealed plastic bag which covered a surgical tray containing a variety of sterilised instruments and other items. Sterilised swabs were then used to clean my chest near my right collar bone and a sterilised syringe was used to punch a hole in my chest, and then a sterilised tube was fed into an artery under my skin and pushed toward my heart. After this procedure was completed the tube was stitched in place with about 6 inches protruding outside of my chest where it divided into 3 branches which were each capped at the end. I was instructed to clean the stitched area each day to prevent infection and that the tubing could then be kept in place for several months during my hospital stay and at home until I had recovered from the treatment. I was then taken back to a private room in the cancer ward.
The reason so much care was taken to prevent infection was because the stem cell transplant and the chemicals completely destroys the immune system so any contracted infection can be fatal. The ward floors and bedding were also thoroughly sterilised and the air was filtered.
Soon after returning to the ward a nurse entered the room and put on a surgical gown and mask and gloves and placed a bag of chemicals on a 6 foot high stand near my bed. A tube from this bag was fed into a machine which regulated the flow of chemicals and then the end of the tube from that machine was plugged into one of the branches of the tube in my chest so that chemicals started entering my blood stream. The nurse then placed another tube on the stand and repeated the process so that 2 bags of fluids were draining into two of the branches of the tube in my chest. The second tube could later carry other chemicals, or nutrients as required by the patient. The nutrients were provided because the chemicals caused nausea and throat ulcers which made it difficult to eat by mouth. The third branch of the tube in my chest was left free so that blood samples could be taken daily, or when required.
Within a few hours of the chemicals being given I became nauseous and began to vomit impulsively and violently which required me to jump out of bed and vomit into a bowl on the right side of my bed, and within a few moments I had sudden diarrhoea which required me to leap frog over the bed and sit on a commode to empty my bowels, and a few moments later I had to get out of bed to urinate urgently. These things happened so suddenly that I tended to get tangled in my tubing and to place strain on the stitches which were holding it in place in my chest.
The problem was compounded by the fact that I had a thin physique and it was summer so I generally felt cold in the air-conditioned wards of the hospital so I wore thermal T-shirts. One was a polo neck and the other had a broad neck. However I had been advised to wear a button up shirt so that the nurses could access the tubing in my chest easily, but I did not have such a shirt with me.
As a result, whenever I moved in the bed the tubing tended to drag on the neck of my T-shirt causing strain on the stitches which held it in my chest. In addition to this, whenever the nurses came to check my tubing or do a blood test they would have to reach clumsily into the neck of my T-shirt to find the tube, and then awkwardly drag the tangled tube out, invariably pulling on the stitches in my chest.
I was also given antiseptic swabs and instructions on how to clean around the catheter insertion site to prevent infection. I had to do it myself, rather than have the nurses do it for me, so that when I left hospital a month later I would be able to keep the wound clean at home. However, because of the side-effects of the chemotherapy my fingers seemed to be slightly numb and not as nimble as usual, and because I was feeling nauseous and ill and because of the position of the tubing in my upper chest I found it difficult, and in fact impossible to bend my neck far enough to look down to see the insertion site directly. Also my eyesight was not good and I found it difficult to see the wound in the mirror because the line across my bifocal lensess was getting in the way, and it was difficult to coordinate the cleaning process because the mirror image is the opposite of the wound. Therefore in my clumsy attempts to clean the skin around the catheter I often felt sharp pain as I knocked the catheter.
Eventually, on the third day I rolled over in bed and the tube pulled on the neck of my T-shirt and dragged on my chest causing it to be sore and within the next few hours I noticed that my T-shirt was getting wet. This was because the fluid was leaking out of my chest at the entry site of the tube. A nurse then came to inspect the tube and noticed that it was leaking, and also that, as a result, my skin was showing signs of infection, so the tube had to be removed.
A specialist told me that this would make it difficult to provide me with intra venous nutrients in the future, and that consequently it would significantly reduce the chances of me making a long term recovery from the cancer.
For various reasons, including my poor condition following the transplant, it was not possible to insert another catheter directly into my chest so several attempts were made to get a different type of tube, called a picc line, into my chest via my arm, but each time the tube became stuck in the armpit area and had to be removed. The only alternative was to insert two tubes, called jelcos into my left wrist and the chemicals were inserted through them.
These tubes presented a few limitations and problems. For example it was not possible to deliver nutrients through them so my only source of nutrition for the next two weeks was vitamin enriched liquid milk mixtures which I forced myself to drink despite the problem of severe nausea. Also the jelco tubes became infected more easily and so were routinely removed each second day and then two new ones were inserted into my right wrist and then plugged into the chemical tubes. This change of tubing occurred every second day for the next month. Also it was not possible to take blood samples from them so an injection had to be inserted into my arm at least once a day for blood tests to be taken. In other words because the one chest tube had to be removed I had to have 60 additional injections in the following month, which were all given while I was quite unwell.
I thought that I might have been able to prevent the problem by not wearing the thermal T-shirts and by keeping myself warm by some other means, and that I could redesign my own T-shirts to overcome the problem if I had to have similar treatment in the future. I also considered the fact that many other patients would have exactly the same problems.
This T-shirt would be a slight modification of my own open neck thermal T-shirt with two cuts down each side of the neck for about six inches so that a flap in front would leave the shirt open with easy uncomplicated and fully visible access to the tubing in my chest. After the tubing had been inspected or used for blood tests the flap could be simply replaced and held in position by moderately secure velcro strips until the next blood test. If the velcro had moderate strength then any pulling or strain on the tubing would tend open the flap and give the patient advance warning so that they could stop rolling in bed before the tube dragged on the stitching in the chest. By this means thousands of patients around the world could avoid the months of inconvenience associated with the removal of the CVC. The improved success rate would also reduce the costs of treatment.
I call this T-shirt design The C-shirt (The CVC or Cancer Shirt) and recommend that it be included in the kit which is given to the surgeon when the tubing is inserted. (The surgeon would get his gown, mask, and gloves, and the patient would get his C-shirt). The benefits would far outweigh the very slight cost, and if this became an accepted idea I presume that I would be entitled to a small royalty for each C-shirt.
Max Banfield
P.S. On previous hospital visits I had become cold due to the hospital air-conditioning, so prior to going on this occasion I packed two of my thermal T-shirts so that I could keep warm and so that, when one was being washed each second or third day, I could wear the other. I also purchased 3 knee length T-shirts which were labeled as ‘one size fits all’.
However I had not had a stem cell transplant or a CVC before so I was unable to predict or prepare for the treatment and I am sure that other patients would have the same problem.
I therefore suggest that the CVC kit include two different sized C-shirts of moderate warmth characteristics to suit most patients and the benefits would still far outweigh the costs. M.B.
How to survive Cancer and Chemotherapy
The INDY formula . . . AAS method . . . RTC’s (which I may explain later)
A brief summary of my experience with cancer1993. Diagnosed with cancer with no hope of a cure and only 2 months to live based on blood tests, a bone marrow biopsy, a surgical biopsy, and the following CAT scan report.
1995? A lump about the size of a tea spoon scoop appeared on the left side of my neck, and grew to the size of a golf ball and remained that size for a long time. It then grew to the size of a hens egg and stayed that size for more than a year. 1998. Surgery to remove that lump from the left side of my neck. Five doses of CHOP chemotherapy given at six weekly intervals where I lived like a hermit to avoid infections, and fatigue nausea and vomiting were regular 2 week features of each cycle of treatment. 1999. Pain in my lower right chest when I inhaled, which made it difficult to breath, and which was due to a fluid build up below my right lung due to cancerous lymph glands in that area. Surgery to remove a cancer the size of a large orange which was wrapped around my ureter and the base of my kidney, and caused it to fill with fluid and swell up. 2-4 weeks rest to recover from the chemo. DHAP chemotherapy which was followed by 3 months of severe nausea, dry reaching, vomiting, and inability to eat properly. A month to recover from the DHAP side-effects. An autologous stem cell transplant followed by 2 weeks in an isolation ward to prevent infection, and four weeks of vomiting in hospital, and six months of vomiting at home. 2 years where food tasted like cardboard, and eating was unpleasant. 4 years where my immune system was depleted which resulted in an infection and dehydration, and hospitalisation where I was treated with intravenous antibiotics and fluids. 2 weeks of recovery. 2004 Complete recovery with no side-effects, no damage to any part of my body, and no after-effects from the treatment except baldness. |
Diagnostic details 1993
In 1993 I had a blood test and was told there was something wrong with my blood. Soon after that I had a CAT scan and was told that there were a lot of unusual lumps in my groin, my abdomen, chest, and neck.
Soon after that I had a bone marrow biopsy and was told there some abnormalities were found.
I then consulted a cancer specialist and told him that I was not interested in reassurance but wanted the plain, objective, scientific facts.
He told me that my body was riddled with cancer, and that I would be dead within 2 month, with no hope of a cure, and that I should tidy up my financial affairs.
I asked him if that was the best or worst case scenario, and he said I might live 20 years. I then began asking questions.
I asked why he thought I would be dead in two months? He then explained that had one small lump in their neck, about the size of a golf ball, and if they cut it out early, and then applied chemotherapy, they could remove the main cancer, and any small amounts which had started to spread. He added that if people had cancers ‘only’ in their chest, or only in their abdomen, there was sometimes success in curing it, but when there were multiple lumps in the chest and abdomen the chances of a cure were slim. He said that in my cause there were lumps in my neck, chest, abdomen, and groin, and the cancer had probably existed for years or even decades and was too late to stop. The best he could do was to send me home and wait until lumps started to block my lungs or my heart, or kidneys, and other vital organs and threaten immediate death. He would then remove them by surgery as each blockage occurred, to prolong my survival. He said that he couldn’t chop all of the lumps out now because there would not be enough of my body left, and the cancer was also in my blood and bone marrow, so I would die anyway.
How and why I survived
I will now give some insight into how I survived the cancer, the surgery, the chemotherapy, and am still alive in 2012, whereas most other people have died.
1. The AD method
2. The diagnosis and treatment was given at the Royal Adelaide Hospital (RAH) which has the reputation of being one of the top cancer hospitals in Australia, and some say it is one of the best in the world, and it is associated with the Institute of Medical and Veterinary Science, and the Hanson Cancer Institute. Many people come from interstate to be treated there. It is only a half an hours drive from my home.
3. I phoned The National Cancer Institute and asked them to send me information about the cancer and side effects in plain English so that I could get a good introduction and basic understanding to the problems. A few days later I received several booklets of information and read them.
4. The RAH has an education unit with staff who discuss the side-effects of treatment, and how to recognise them before the treatment starts, and what to report and do about them. They are also accessible for phone enquiries.
5. The RAH also has a social work department with staff who solve some of the problems of how to get to hospital when you are too ill to travel by bus. For example it is not practical to go to and from the hospital by buses or other public transport, because vomiting is a side effect of chemotherapy. Hence the nurses provided vomit bags and social workers arranged for car and ambulance transport when necessary.
6. I was instructed to have blood tests (I think every month), and CAT scans and consultations with a cancer specialist every three months, and a bone marrow bone marrow biopsy every 12 months. I was also told to report any lumps or other symptoms immediately because the purpose of the monitoring was to catch the cancer as soon as it changed from low grade to high grade. I was advised that immediate treatment at that stage would stop the cancer before it blocked major organs, and before it spread out of control. A physical examination to check for internal lumps, and blood pressure was measured at each 3 monthly consultation,.
7. When I was told I had only 2 months to live I was not concerned because I didn’t have any symptoms at all, and because in my personal experience doctors had been wrong with their diagnosis in the past. I therefore have a ‘wait and see’ attitude, and a ‘don’t assume the worst’ approach. I decided that if I was dead in 2 months the diagnosis would be correct, and if not, it would be wrong. In other words – don’t panic unnecessarily. I also had a lot of other health problems so I didn’t care anyway. i.e. If I was going to die – let it be.
8. After 2 months passed I thought – that was lucky, and then five months passed, and I suppose I wrote my will within a year. During that time I did some reading on the subject and came to a very causual conclusion that I had a life expectancy of 2 years, and at the most five years.
9. I didn’t want anyone to know I had cancer because I didn’t want it to have an adverse effect on my personality by having people come up to me all day and pity me. Consequently, I only told about 3 people in the first six years, and only about six in the entire period. Essentially their role was to come and get me if ever I was too sick to get out of bed and get to hospital on my own etc., or to do the shopping if ever I was too sick to do it myself which rarely happened.
10. About six years went by when a small lump, the size of a golf ball, appeared on the side of my neck, and stayed that size for about 18 months. It wasn’t removed because a blood test confirmed that the cancer was still ‘slow growing’, and treatment was only given when it was ‘fast growing’. The idea was that the chemo was only effective at killing fast growing cells such as the hair, finger nails, and cancer, and could be stopped before it killed too many of the the slow growing cells of your body, and then the cancer would be gone, and your body could recover.
11. After a few years went by I became aware of some of the fringy frootloop theories, and none of them seemed sensible to me, but I was going to die anyway, so I had nothing to lose. One of them was aimed at starving for long enough to see the cancer die, and then outlive it and start eating six weeks later to recover. I decided that there was not real risk because I could stop anytime, and I could use the lump on my neck as a guage of it’s effectiveness. i.e. If the lump went down the diet would be killing it, if not, the diet was useless.
I had absolutely no food for four weeks, and lived solely on about half a dozen one litre bottles of mixed fruit juice potions per day,
After about a month I was becoming weak, and getting worse, and the lump was the same size, so the diet wasn’t working, and I abandoned it.
While I was starving every piece of food looked delicious, but I couldn’t eat it, and when I stopped the diet I went to a cake shop and stuffed my face full of cakes and scones etc. I also had a cup of coffee, but the milk seemed off, and I contracted severe food poisoning and starved and vomited from another week because I was simply too sick to eat. and then I recovered. The vomiting may have been induced because I put too much food into my starved stomach too soon, or because of the milk was old and off. It was the last of about 2 of the fingy nonsense methods that I tried.
The experience gave me confidence in the durability of my body in harsh circumstances.
When I was going through the most severe side effects of chemotherapy, I looked upon it as a situation in which the rich, healthy, and privileged people of the world had to climb Mount Everest to seek a challenge, and test their courage and their limits of endurance, and prove themselves, and gain confidence, whereas I didn’t have to go anywhere to deal with the greatest challenge anyone is ever likely to experience.
To be continued . . .
The nausea side-effect from chemotherapy
The worst side-effect that I had from CHOP chemotherapy was nausea for about 2 weeks of each of five sessions of chemo given over six months. The worst side-effect from DHAP chemotherapy was many weeks of dry reaching. The worst side-effect from the stem cell transplant was six months of nausea and vomiting.
The medication prescribed to treat the nausea were not very effective, and one of them caused a very common side-effect which was an annoying aching of my shoulders and hips which was worse than the nausea, so i stopped using the anti-nausea medication very early in the treatment processes.
The most common side-effects for stem cell transplants are pain, particularly caused by throat ulcers, and nausea. In fact I was told that virtually all patients had so much pain that they were all given a morphine machine attached to their wrists by a tube into their veins so that they could administer the pain killing drug in small doses themselves, any time they wanted for 2 weeks following treatment.
In my case three doctors examined the ulcers in my throat, one after another, and each of them took turns trying to persuade me to stop acting like a hero and accept the morphine machine to help with the pain. I told them that I didn’t have much pain, and let them give me one small injection to see what happened. It didn’t make any difference, so I didn’t have any more injections, and was not attached to the machine.
In fact, the reason those doctors were so concerned was because they looked into my mouth and could see a massive amount of fungal infection in my throat, but the only time I felt any pain was when I tried to eat, because it felt as if the food was passing through a tangled mess of razor blades in my throat.
I naturally tried to eat, but found it extremely difficult, and even if I managed to get it into my stomach, it usually came out as vomit immediately, or within a few minutes. At times, I was either vomiting, or passing diarrhoea, or urinating almost every fifteen minutes. The only nutrients that I was able to consume effectively was small cartons of flavored milk, or small cans of vitamin enriched liquid food.
Although I didn’t have much difficulty dealing with the pain, I continued to have extreme problems with nausea. For example, freshly cooked meals would be delivered to the ward three times a day, and I would feel like vomiting, just from the smell of it, as soon as it came through the door fifteen feet away, At other times I would feel nauseous as soon as the food was placed on the platform at the end of my bed. I would also vomit just from the smell of plain tap water because I could smell whatever normal chemicals were in it, such as chlorine. By contrast, there was another man who did not appear to be affected by nausea, and he could eat greasy fish and chips without any problems.
While I was having those problems I would ask other patients and neighbours how they relieved them, and for the most part nothing much was useful, so I just had to tolerate the symptoms until they were over.
On one occasion an elderly neighbour saw me staggering down the street, and asked me what the problem was, She then invited me into her flat and said that she had found that a drink of brandy and dry ginger had given her some relief, and hen she gave me a drink. It did provide some very mild relief of nausea. From that day onwards she would always invite me in for a drink each time she saw me walk past.
I recently saw a comment on Twitter about the beneficial effects of ginger for chemotherapy and nausea with a link to a website here.
Several other patients recommended that I try marihuana, but I never did, so I don’t know if it would be effective or not.
However, I do not wish to be a drug addict, so even if I did try it, I would only use it for as long as required for the purpose of relieving nausea,
Exercise and cancer treatment
(This item was written on 8-8-12, about 8 years after I had surgery, chemotherapy, and a stem cell transplant to treat Non-Hodgkin’s lymphoma.)
While I was being given chemotherapy for cancer I was often so ill that I would rather stay in bed, because the effort of getting out was too difficult, and all I wanted to do was rest.
However, I drew a reasonable conclusion that while the toxic chemicals were in my body they would be having toxic affects beyond what they were intended for, and that the best thing to do would be to exercise to get my blood flowing through my kidneys to flush them out as quickly as possible.
Consequently I did the following things while watching other patients reading books, or watching TV in bed all day
I would walk the length of two wards about three to five hundred times a day, sometimes in the morning, and then having a rest, and then again in the afternoon, and then again in the evening.
On one occasion I had surgery to remove a 5 cm cancerous tumor from my neck. The night before I asked if I could leave the hospital and walk the streets during the Adelaide festival of arts. I explained that the operation was on my neck and not my feet so it should be okay. I walked down Rundle mall and obtained some free tickets to a show, and then walked a mile to the casino to spend about half an hour on the poker machines. When I returned to the hospital the nurses were surprised because they thought I was afraid of the operation and went home to avoid it.
I had the operation the next morning, and the same evening I walked down the mall and attended the free show, and went to the casino again to play the poker machine for a short time, and then returned to the hospital. I was discharged from the hospital and returned home the next day.
On another occasion I had an operation on a 10 cm. diameter cancer that was blocking my left kidney, and had a few problems in the next 2 or 3 days, and was then transferred to an out-hospital for about a week. It was near Semaphore beach so I went for a 100 yard walk to look at the beach and the sea. The next morning I walked about half a mile to the library, and then about 5-10 km along the beach and back, and did that for a few days until I was discharged from the hospital and went home. On one occasion, about 2 weeks later I overdid the exercise, and strained the scar, and felt a rip internally, accompanied by some symptoms which indicated that the injury was probably followed by an adhesion.
While I was at home I walked at least 2 hours per day, at least three, or up to seven days per week, especially in the years when I had cancer, but was not being given surgery or chemotherapy.
However, I had to be practical, and I have to say that there were many times, sometimes for months at a time, when I was so ill from the chemotherapy, that all I could do was stay in bed, or get out and crawl about, or more or less just stagger along the street.
I always thought that I had to be in my best condition before I got smashed about by the toxic affects of the chemicals again.
Some more information on my diet and exercise in relation to heart disease and cancer is dicussed in my iTunes talk available here.
Diet and infection avoidance during chemotherapy
(added 4-10-2012 and improved later)
Shortly before being treated with CHOP chemotherapy I was advised that chemotherapy impairs the immune system, and that I should avoid crowds, and also avoid eating at restaurants where food might be contaminated, and to avoid buying the type of foods which are more likely to be a source of infection. For example, I was told not to eat lettuce.
I took that advice for the six months of treatment, and essentially lived like a hermit, with instructions to my friends not to visit me until after I survived. I treated the whole process as a challenge, and would walk slowly to the shops, and when I was within ten feet of the doors I would wait until they opened and rush briskly to the greengrocers and through the supermarket, and not slow that process except when absolutely necessary, until I was outside again, and 10 feet from the door, and then I would walk slowly home.
I was given the same advice when the cancer returned 18 months later, and before I started DHAP chemotherapy. However, the previous instance involved a lot of social isolation, and during DHAP I did occasionally attend social events.
Soon after that, when I was being treated with a stem cell transplant I was kept in an isolation ward for two weeks to avoid infection, and was given some nutrients intravenously, and the food was prepared by the hospital, and specifically chosen because it was the type which minimised the risk of infection.
The floors and bedding were kept clean, the air was filtered , and I was advised to shower regularly and to keep the catheter insertion sites clean, and I asked my friends not to visit me until the treatment was over.
Despite that a catheter entry site became infected, and I was given intravenous antibiotics to treat it.
I may give more information on my diet and infection avoidance methods later.
Fats in the diet
When foods such as grains or vegetables are sprayed with pesticides and are then eaten by animals, the toxic chemicals tends to deposit in the fatty tissue of their bodies, and, consequently, as those animals grow older they build up in larger concentrations, and then, when the people consume lamb and beef they tend to consume higher quantities of those chemicals in one serve.
Therefore a good way of preventing cancer would be to eliminate toxic chemicals from the diet by eating foods which have been grown in the natural way without pesticides
It would also be an advantage to eliminate fatty meats from the diet.
In other words people who consumed a natural or organically grown vegetarian diet would be more likely to lead a healthier, cancer free, and longer life,
Cause and prevention of NHL
There have been some studies which link Non-Hodgkin’s lymphoma to previous infections with the Epstein-Barr virus which I was aware of before I was diagnosed, and I had considered various possible viral causes so it didn’t completely surprise me.
About 2 weeks before bladder surgery in 1993 I took aspros to relieve some mild neck ache and prevent it from becoming a problem when I went into hospital, and then a neighbor, who had previously been a nurse advised me to stop, because that drug thins the blood and can slow down the healing of surgical cuts.
Furthermore the aspro stays in the blood for two or more weeks.
I also had a flu immunisation injection to prevent the flu while I was in hospital (I prefer to be dealing with one problem at a time properly, not 2).
After the operation I was sore in the internal scar area and walked in a slightly bent position to avoid it, but I was told to ignore the pain and stand up straight and walk properly. When I did that I was walking in pain. Soon after returning to my bed I noticed that the urine which drained into my catheter bag was turning dark red to black, indicating that I was bleeding internally and that the blood was mixing with the pale urine.
Another patient in the ward had pale urine in his bag and I asked him about it. He said that he spoke to an uncle before the operation, and was told that he had taken aspirin, and bled a lot, and advised against it. That patient did not take aspirin, did not have thin blood, and did not bleed internally.
The thick bloody urine in my bladder soon formed into blood clots which blocked the flow of urine several times. Each time I had to go through the very painful process of having those plugs of blood forced back into the bladder to relieve the blockage. It was done by giving me a morphine injection for pain, and then placing a syringe full of fluid into the catheter and punching it forward to dislodge the blood clot.
By the second or third day I contracted a urinary infection.
I was also having daily blood tests, and within a week I was told that my blood had something wrong with it and needed to be investigated further, after I left the hospital
I then had a CAT scan, and a bone marrow biopsy, which confirmed that I had Non-Hodgkin’s Lymphoma.
Hence the many possible causes include a previous virus, or one or more factors in the combination of aspirin, flu immunisation, blood loss, and blood infection while I was in hospital. The combination of an infection while I was producing new blood to offset the lost blood would seem to be a plausible cause of Non-Hodgkin’s Lymphoma which is a type of blood cancer.
See a more recent report showing the link to the Epstein Barr virus here.
The Public image and cancer survivors
On the ABC TV show called the Gruen Planet of 5-9-12 a group of panelists discussed world champion cyclist Lance Armstrong, and the accusation that he had used sports enhancing drugs to enable him to win 7 Tour de France titles.
The general question was what effect the accusation of being a drug cheat would have on his public image.
On the positive side was the fact that he had previously been diagnosed with testicular cancer, which had spread to his lungs and brain in 1996, and yet he managed to survive and return to racing.
His public image was enhanced by that fact, as well as his efforts in raising more than five hundred million dollars toward research to help the other 27 million cancer patients.
The two opposing views were that his survival and his fund raising were worthy of respect because it gave many other people the hope that they too would survive, and that it outweighed any adverse impact caused by the drug cheating accusations.
The negative view was that he had cynically used the fund raising as a means of offsetting any effects of his drug cheating if he was ever found guilty.
When I joined Wikipedia to add useful information about health problems which would help millions of other patients, I was accused of being a non-notable fringy kook, and when I was asked to tell the other editors more about myself to clear up any conflict of interest allegations, I didn’t know what else they wanted, or needed to know, so I mentioned that I was diagnosed with cancer in 1993. One of the editors then accused me of being a liar, but did not specify what I was supposed to have lied about, and left the impression that I was telling lies about having cancer.
I was diagnosed as having a form of cancer called Non-Hodgkin’s lymphoma, and told that it had spread to my blood, my bone marrow, and the lymph glands of my chest and abdomen, and I was given two months to live with no hope of a cure in 1993, three years before Lance Armstrong. Surgery and treatments started in 1998, and finished with a stem cell transplant in 2000.
The only thing that I can say in a manner that is objective and factual, is that I am still alive in 2012, and that two editors were trying to defame me, and destroy my public image inside of Wikipedia, in order to get me banned. e.g. See one of my reports here.
I was diagnosed with cancer and given two months to live with no hope of a cure in 1994, but a lot time went by and many things happened after that, and ultimately a stem cell transplant in 2000. Four years later I was still having varying degrees of side-effects when I rang my doctor and said that I was too exhausted to attend an appointment and would see him again in a week. He insisted that I phone an ambulance and go to hospital, and I said that I was too exhausted to do that, and after three or more times I finally agreed. About an hour later I heard a knock on the door, and then crawled from my bed to the door.
I looked up at the handle and wondered how I would get the energy to stand up and open it, and after about six attempts I made one final, and extremely difficult, and lucky leap, and caught the handle. I opened the door, and saw two people in ambulance uniforms. The trip from the door to the ambulance and then to the hospital was also difficult, but I made it, and survived a week of treatment, and another two weeks at home before making a complete recovery, and haven’t had any problems since.
I can remember what happened as clearly as if it was yesterday.
I suppose it is that old story – when opportunity knocks – take it, because opportunities like that don’t happen very often.
Why I decided to have a stem cell transplant for cancer
By the time I was told that I would need to have a stem cell transplant for cancer, I had already been through six months of CHOP chemotherapy, eighteen months earlier, and had just been through three months of DHAP chemotherapy, and I had seen other people go through chemo and the side effects and die, so I knew of the potential outcomes.
Consequently I had two choices.
The first was to go through the transplant procedure and the potential side effects, with the small possibility of surviving.
The second was to not have the transplant, and wait for the cancer to get worse and produce the severe cancer symptoms, and die a painful and distressing death, with no hope of a cure.
I made my decision on the basis that it didn’t matter what choice I made, the consequences were not going to be pleasant, so I considered in favor of the transplant. As they say it was “the lesser of two evils“.
I also took into account that the side effects didn’t start until a few hours after the chemicals were inserted into my veins, so after that was started the course was set.
There were a lot of problems but I am still alive 19 years later, and haven’t had any significant symptoms or side effects since 2004, i.e. for the most recent eleven years.
The only obvious remnant is that during CHOP and DHAP chemotherapy my hair became thin and grew thick again, and during the stem cell transplant I went bald and now my hair is so thin and spars that it is better to keep my head shaved.
Research information
I have recovered from many serious diseases, and one of my methods is to look for information about people who survived to determine what they did which was different from those who didn’t. For example, I also had angina heart disease in 1997, while I had cancer, and read a book about how Nathan Pritikan survived for 20 years by using a vegetarian diet, so I made some slight modifications to that diet to suit my requirements and treated it successfully. That diet may have assisted in curing the cancer. However, during the periods of chemotherapy the immune system is impaired by the chemicals, so it is necessary to avoid eating some vegetables, such as lettuce, which tends to have bacterial contamination, and to avoid eating at salad bars in restaurants for the same reason.
Also, I did a lot of walking as a form of exercise but I noticed that most of the other patients were laying in bed all day. Of course there were many months when I was too exhausted to do anything, but when ever I was able I walked, sometimes for 100 yards, or 400 yards, or for two hours or more a day.
I don’t know if those facts are responsible for my recovery or not, but they were two of the main things that I did which were different.
For more information about the diet see here